FAQ about keratoconus

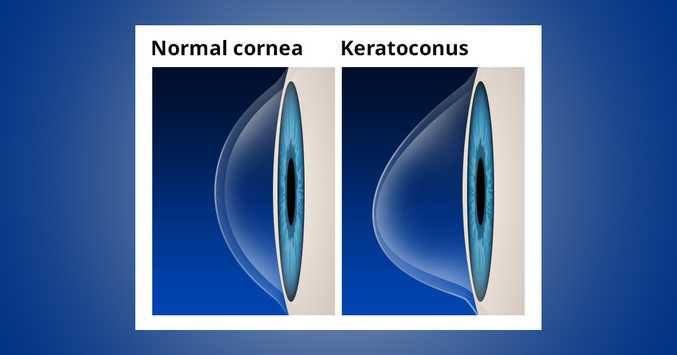
This is an unusual condition in which the cornea of the eye (the clear anterior part of the eye) becomes very thin and projecting. It literally means: a cornea that appears in a conical shape. This distortion may cause serious visual disturbance.
What causes keratoconus?
Despite ongoing investigations, the cause remains unknown. Although it is considered an inherited disease, the probability of homozygous relatives showing keratoconus is considered to be one in ten. Strong eye scarring, although not considered a cause of the keratoconus, can contribute to pathological development. Therefore, patients with keratoconus will be good to avoid rubbing their eyes.
What are the symptoms of keratoconus?
The first symptoms are blurring and distortion of vision. Symptoms usually appear late in adolescence or early in the first 20 years of life. Often the keratoconus develops slowly for 10 or 20 years and then stops. In the early stages, vision may be disturbed slightly, causing blur, photosensitivity and irritation. Every eye is affected to a different extent. As the disease progresses and the cornea becomes curved, vision is disturbed accordingly. If the cornea is swollen, the visual acuity may suddenly decrease. The cornea exits when the elastic portion presents a small crack caused by its continuous stretching due to the projected conical structure. Swelling can persist for weeks or even months as the crack heals and is gradually replaced by scar tissue.
How is the keratoconus treated?
Light cases are treated with glasses or special design contact lenses. When vision is no longer satisfactory with glasses or contact lenses, surgical treatment of keratoconus is recommended, keratoplasty as it is called.
A new method for treating keratoconus that can reduce the need for semi-contact contact lenses or for transplantation is the use of infrared light (UVA). This technique called “Corneal collagen intercourse” or “Collagen Crosslinking with UVA-Riviflavin” treats the keratoconus by collagen polymerization thus “freezing” its evolution. The main goal with this treatment is the stabilization of the corneal shape, ie the retention of the keratoconus.